Radiation Isolation for Radiation Therapy Patients: Best Practices
Radiation therapy is a crucial treatment modality for individuals battling cancer. While it is effective in targeting and destroying cancer cells, it is essential to prioritize radiation isolation to ensure the safety and well-being of both patients and healthcare professionals. In this article, we will discuss best practices for radiation isolation during radiation therapy, providing valuable insights and guidelines for a safe treatment experience.
Contents
- 1 Understanding Radiation Therapy
- 2 1. Communication and Education
- 3 2. Designated Treatment Area
- 4 3. Restricting Visitors
- 5 4. Personal Protective Equipment (PPE)
- 6 5. Monitoring Radiation Exposure
- 7 6. Handling Radioactive Materials
- 8 7. Proper Waste Management
- 9 8. Maintenance of Equipment
- 10 9. Patient Comfort and Support
- 11 10. Follow-Up and Monitoring
- 12 Frequently Asked Questions
Understanding Radiation Therapy
Radiation therapy is a specialized treatment that uses high-energy radiation to target and destroy cancer cells. It is a precise and effective treatment option for various types of cancer. However, due to the nature of the treatment, precautions must be taken to protect individuals from unnecessary radiation exposure.
1. Communication and Education
Clear communication between patients and their healthcare providers is vital during radiation therapy. Patients should receive comprehensive education about the treatment process, its goals, potential side effects, and safety measures. Understanding the importance of radiation isolation and following the instructions provided by the medical team are crucial for a successful treatment experience.
2. Designated Treatment Area
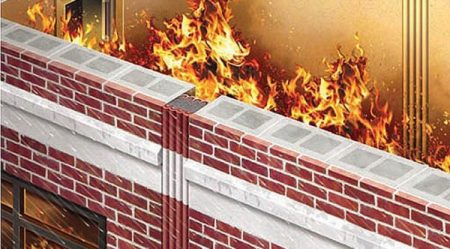
Patients undergoing radiation therapy should have a designated treatment area that is separate from other living spaces. This area should be properly shielded and equipped with necessary safety measures to prevent the spread of radiation. It is important to minimize the time spent in this area to reduce unnecessary exposure to radiation.
3. Restricting Visitors
To ensure radiation isolation, it is essential to restrict the number of visitors in the designated treatment area. Only authorized personnel, such as healthcare professionals and caregivers, should be allowed in this space. Visitors should adhere to safety protocols and wear appropriate protective gear, as advised by the medical team.
4. Personal Protective Equipment (PPE)
Healthcare professionals working with radiation therapy patients should wear appropriate PPE to minimize their exposure to radiation. This may include lead aprons, gloves, and leaded glasses. Proper training and adherence to safety protocols ensure the effective use of PPE and reduce the risk of radiation exposure.
5. Monitoring Radiation Exposure
Regular monitoring of radiation exposure is crucial for both patients and healthcare professionals. Dosimeters and other radiation monitoring devices can measure the amount of radiation received and help ensure that exposure remains within safe limits. These measurements assist in adjusting treatment plans and optimizing radiation therapy.
6. Handling Radioactive Materials
Radiation therapy involves the use of radioactive materials. Proper handling, storage, and disposal of these materials are essential to maintain radiation isolation. Healthcare professionals should follow established protocols and guidelines to ensure the safe handling of radioactive substances.
7. Proper Waste Management
Strict protocols for the management of radioactive waste should be in place. Proper segregation, containment, and disposal of waste materials contaminated with radiation are necessary to prevent contamination and minimize the risk to both healthcare workers and the environment.
8. Maintenance of Equipment
Regular maintenance and calibration of radiation therapy equipment are crucial to ensure accurate and safe treatment delivery. Healthcare facilities should adhere to strict quality assurance programs to maintain the highest standards of radiation therapy and minimize the risk of errors or malfunctions.
9. Patient Comfort and Support
Providing a comfortable and supportive environment for radiation therapy patients is essential. Emotional support and open communication can help alleviate anxiety and promote a positive treatment experience. Addressing patients’ concerns and providing information about the safety measures in place can enhance their confidence in the radiation isolation protocols.
10. Follow-Up and Monitoring
After completing radiation therapy, patients should undergo regular follow-up visits for monitoring and evaluation. These visits allow healthcare providers to assess the effectiveness of treatment, monitor any potential side effects, and address any concerns or questions patients may have.
Frequently Asked Questions
Q1: Why is radiation isolation important during radiation therapy? A1: Radiation isolation is crucial during radiation therapy to minimize unnecessary radiation exposure to patients, healthcare professionals, and the general public.
Q2: What is the role of personal protective equipment (PPE) in radiation therapy? A2: PPE, such as lead aprons, gloves, and leaded glasses, helps protect healthcare professionals from radiation exposure during patient treatment sessions.
Q3: How is radiation exposure monitored during radiation therapy? A3: Dosimeters and other radiation monitoring devices measure the amount of radiation received by patients and healthcare professionals, ensuring exposure remains within safe limits.
Q4: What are the best practices for handling radioactive materials in radiation therapy? A4: Strict adherence to protocols for handling, storage, and disposal of radioactive materials is essential to maintain radiation isolation and prevent contamination.
Q5: What happens after completing radiation therapy? A5: After completing radiation therapy, patients undergo regular follow-up visits for monitoring and evaluation to assess treatment effectiveness, monitor side effects, and provide ongoing support.